September 01, 2022
Soon after Maranda Douglas gave birth to her daughter in April of 2018, she started having persistent lower back pain. Over a 10-month timespan, the pain got worse. Maranda ended up in the emergency room when the pain became unbearable. A CT scan revealed that Maranda had Desmoid tumors. While technically noncancerous, Desmoid tumors are growths that occur in the connective tissue and can be very invasive, painful and affect nearby organs.
Finding Dr. Goodwin 
Maranda and her mom began researching and found an oncologist specializing in Desmoid tumors in New York. In March of 2019, they traveled for a consult and were told he "had never seen a case quite like Maranda" because of the amount of and size of tumors: They spread from her breasts to her lower back. He wanted Maranda to start chemotherapy and referred her to Dr. Van Tine at the Siteman Cancer Center in St. Louis.
In March of 2020, Maranda's pain worsened, accompanied by weakness and numbness. Now with pain, weakness, difficulty moving and a large tumor in her spine, she was referred to Matthew Goodwin, MD, PhD, a spine surgeon with Washington University Orthopedics.
First Visit of Many
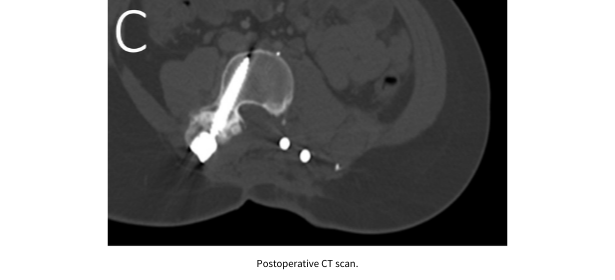
 On her first visit, Dr. Goodwin showed her the scans and X-rays and pointed out that the tumor on the left side of her spine had gotten so large so fast that it had eaten holes through her spine. “It was very shocking because I hadn’t realized the tumors had grown that fast…I needed surgery immediately!” Maranda says.
On her first visit, Dr. Goodwin showed her the scans and X-rays and pointed out that the tumor on the left side of her spine had gotten so large so fast that it had eaten holes through her spine. “It was very shocking because I hadn’t realized the tumors had grown that fast…I needed surgery immediately!” Maranda says.
Dr. Goodwin says, “Anytime an oncologist like Dr. Van Tine calls you to tell you about a patient with a large and aggressive tumor in the spine, you prepare for it to be large and aggressive. Maranda's was just that: a big, aggressive tumor that was growing even bigger, very rapidly. It was the size of a small basketball, destroying bone and pushing on the nerves to her leg.”
“In order to remove a tumor of this size it really is a team effort. Because it was so large, she was going to be left with a big hole in her back and flank once I removed it. Luckily, we have a microvascular team, Drs. Boyer and Brogan, which specializes in providing soft tissue flap coverage for cases like this. These cases can’t be done without their expertise to help fill in and ultimately heal the hole I create.”
All-Day Surgery
On April 20, 2020, Maranda underwent an all-day surgery at Barnes-Jewish Hospital that included resection of the tumor with parts of her spine, reconstruction of her spine, and harvesting of a muscle flap that was then used to close the wound. 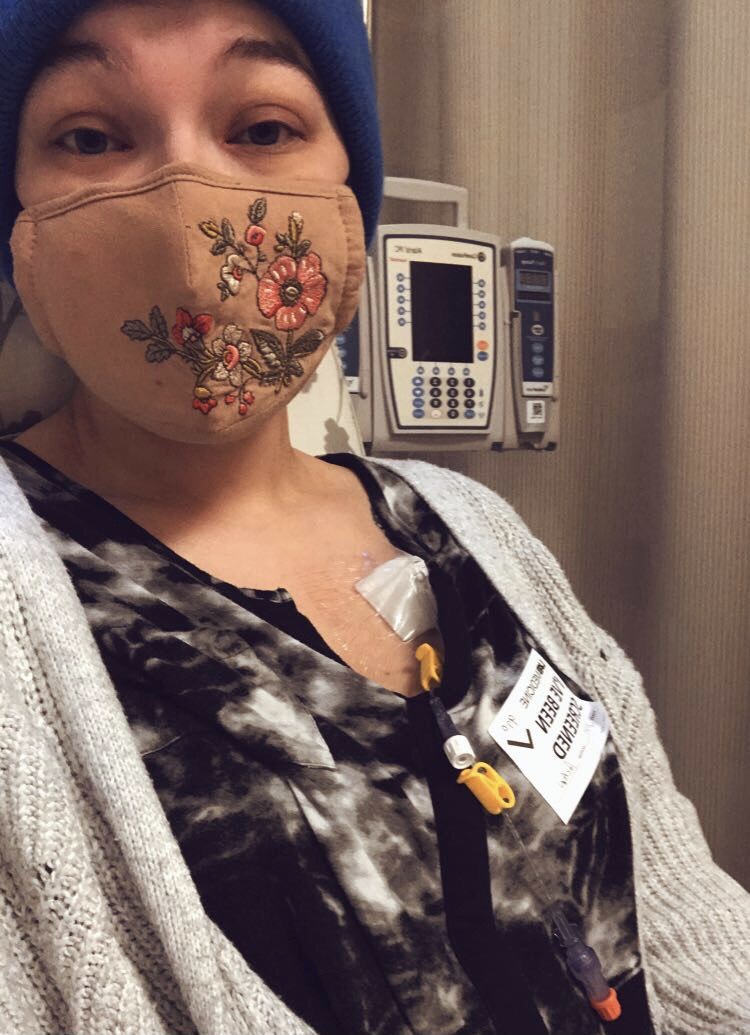
Dr. Goodwin explains, “Maranda’s tumor was pushing on her spine and had eaten through the bone in many places, requiring an extensive resection and reconstruction with rods and screws, but with careful dissection around the nerve roots going to her legs.” Despite the large-scale nature, Dr. Goodwin says Maranda did great and had immediate relief of pain in her leg.
“Maranda has been one of my favorite patients because while she has these terrible tumors, she remains so incredibly kind, and incredibly tough. As I have gotten to know her, I realize I have to really pry when I ask her if anything hurts, because she downplays everything. They don’t come any tougher than her.”
“I woke up from surgery scared and overwhelmed,” Maranda remembers. “I didn’t know what recovery was going to be like or how it would affect me. Due to COVID-19 restrictions at the time of her stay, Maranda spent eight days without friends or family - five of those days in the ICU. She had to lay on one side to keep the pressure off of the soft tissue flap, but was able to get up and sit in a chair two days after surgery. She recalls her care team being impressed with her progress at sitting in a chair so soon.
“Almost instantly I could feel the huge difference in my body with the tumor removed. I expected a little pain from surgery, but the previous, severe pain was gone. I had no more nerve pain,” Maranda says.

Looking Up
Once released, Maranda started a new round of chemotherapy and physical therapy. She laughs and says, “We had a lot going on, dealing with four drains and dressing changes every day. It was definitely a learning experience - my dad and step mom are not doctors.” She says they also had to keep up with several prescriptions, but pain medication was not one of them. “I was sent home with two weeks’ worth of pain pills and I did not even need the whole two weeks.”
Perfecting Posture
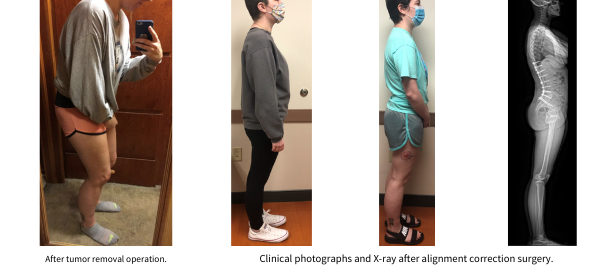
Dr. Goodwin shares, "This tumor was quite large and had been pushing on her spine, eroding it. After I resected it, the curvature of her spine changed some, making it difficult for us to recreate her prior curvature. As a result, while her tumor was out and her legs regained function, she was leaning forward some. After a few months of therapy I told her we could make her alignment better, but like most things, she wanted to work harder in therapy to fix it! Finally, after 9 months she agreed she would like her alignment to be better and we returned to the OR to recreate her alignment. She did great with this and her spine and posture looked fantastic afterward."
.png)
To This Day...
 Maranda’s recovery has gone well, she has full strength in her legs and is much more mobile. Though she and her family have since moved to Alabama, she has not transferred her care. Instead, she makes the trip to see Dr. Goodwin and Dr. Van Tine in St. Louis.
Maranda’s recovery has gone well, she has full strength in her legs and is much more mobile. Though she and her family have since moved to Alabama, she has not transferred her care. Instead, she makes the trip to see Dr. Goodwin and Dr. Van Tine in St. Louis.
Maranda says, “My appointments with Dr. Goodwin may be two-hours long because he is thorough and takes the time to answer all of my questions. I could not have asked for better medical teams and surgeons. They treat you with such care!”