May 12, 2022
The Department of Defense (DOD) funds the Peer Reviewed Orthopedic Research Program (PRORP) for innovative, high-impact, clinically-relevant research to advance treatment and rehabilitation from bone, muscle and joint injuries sustained during combat-related activities. At Washington University Orthopedics, we are doing our part to contribute to the research that leads to a better quality of life for injured service members.
Survivor Needs
The advances of medicine have fortunately saved and/or resuscitated service members involved in once-fatal accidents. The positive increase in survivorship has increased the number of service members and veterans living with injuries sustained to their extremities. Combat-related orthopedic injuries are often distinctly different from those in the civilian setting since they more frequently involve multiple-limb trauma, open fractures, major tissue loss and a high degree of wound contamination. Also, these injuries are often sustained in harsh environments where optimal care access can be limited.
Over half of all combat injuries sustained during Operation Iraqi Freedom and Operation Enduring Freedom were extremity-related injuries and orthopedic-specific conditions, representing the largest source of long-term disability in service members.
Since 2009, the PRORP has dedicated its Congressional allocations of $368.5 million to supporting military-relevant orthopedic research that also benefits the treatment and care of the general population.
John Clohisy, MD, and Matthew Silva, PhD, are leading research investigations with the goal of discoveries, developments, and applicable healthcare solutions for Service members, Veterans, and the American public.
Dr. Clohisy's Research: Relieving Pain and Preventing Osteoarthritis
 John Clohisy, MD, the Daniel C. and Betty B. Viehmann Distinguished Professor of Orthopaedic Surgery, is researching improved clinical outcomes of femoroacetabular impingment (FAI) surgery with a Department of Defense grant. Femoroacetabular impingement (FAI) is a condition of the hip characterized by abnormalities of the acetabular rim (hip socket) and the femoral head/neck (hip ball) region. With hip motion, the femoral head and neck “bump” the acetabular rim, and over time this repetitive contact injures the hip joint, causes pain and leads to secondary osteoarthritis (OA).
John Clohisy, MD, the Daniel C. and Betty B. Viehmann Distinguished Professor of Orthopaedic Surgery, is researching improved clinical outcomes of femoroacetabular impingment (FAI) surgery with a Department of Defense grant. Femoroacetabular impingement (FAI) is a condition of the hip characterized by abnormalities of the acetabular rim (hip socket) and the femoral head/neck (hip ball) region. With hip motion, the femoral head and neck “bump” the acetabular rim, and over time this repetitive contact injures the hip joint, causes pain and leads to secondary osteoarthritis (OA).
This disorder commonly affects military personnel and young active individuals in the general population, but also affects middle-aged and elderly patients as the disease progresses and OA develops. In fact, FAI is thought to be the most common cause of hip OA. Recent research has shown that 87% of active military personnel with hip symptoms have FAI. This condition can restrict military personnel function during active duty, cause long-term disability, and increase the risk for hip OA and total hip replacement in our active duty, veteran and general populations.
FAI is the most common hip condition in patients younger than 50 years of age. These patients are commonly active and athletic and develop hip symptoms over time. Equally important is the association of FAI with the eventual development of hip osteoarthritis. As the risk for hip osteoarthritis and the need for total hip replacement continues to increase in the general population, the need for preventive treatments magnified.
This condition is currently the focus of intense interest directed at surgical treatment to relieve pain, enhance function and delay or prevent OA. Despite our improved methods of diagnosis and treatment, many patients fail to receive an accurate diagnosis and/or an optimal result from surgery. Currently, there is a major need to improve FAI treatments to provide more consistent outcomes in affected patients.
Addressing an Urgent Need
To develop improved FAI treatments, Dr. Clohisy's research will identify predictors of FAI surgery outcomes. Young patients with symptomatic, pre-arthritic FAI will be studied. This patient population is most commonly between 14 and 40 years of age, is highly active and has hip pain and limitations due to FAI. His studies will be performed by the Academic Network of Conservational Hip Outcomes Research (ANCHOR) study group, and will include two patient groups (cohorts). The first cohort had surgical treatment of FAI between 2008 and 2012 and will be followed at a minimum of seven years. The analysis of this established ANCHOR cohort will have rapid impact on contemporary FAI treatment. The second cohort will be new and characterized by novel imaging techniques, standardized arthroscopic procedures and contemporary outcome measures. This second cohort will provide novel clinical evidence and guidance to optimize future surgical treatments
There is an urgent need to focus on improved FAI treatments given the major burden of the disease. These studies will propel the field forward by improving diagnostic approaches, identifying predictors of surgery outcomes and by determining ideal and individualized surgical techniques. Improved treatment of these disorders will improve the health of all patient populations.
This DOD study results from a unique, multi-center (the ANCHOR study group) to improve the treatment of hip disease in all patient populations. The ANCHOR collaboration was initiated in 2007 and has grown to include 38 surgeon investigators at 19 institutions. Dr. Clohisy is the principal investigator of the group, and Jeffrey Nepple, MD, MS, serves as the co-investigator for this grant.
“Our research team is honored to be funded by the DOD as this opportunity provides potential to improve FAI treatments in military personnel as well as the general population. This condition affects many young troops and veterans, so we hope our work improves the lives of these very dedicated individuals,” Dr. Clohisy shared.
Dr. Silva's Research: Healing Fractures Properly
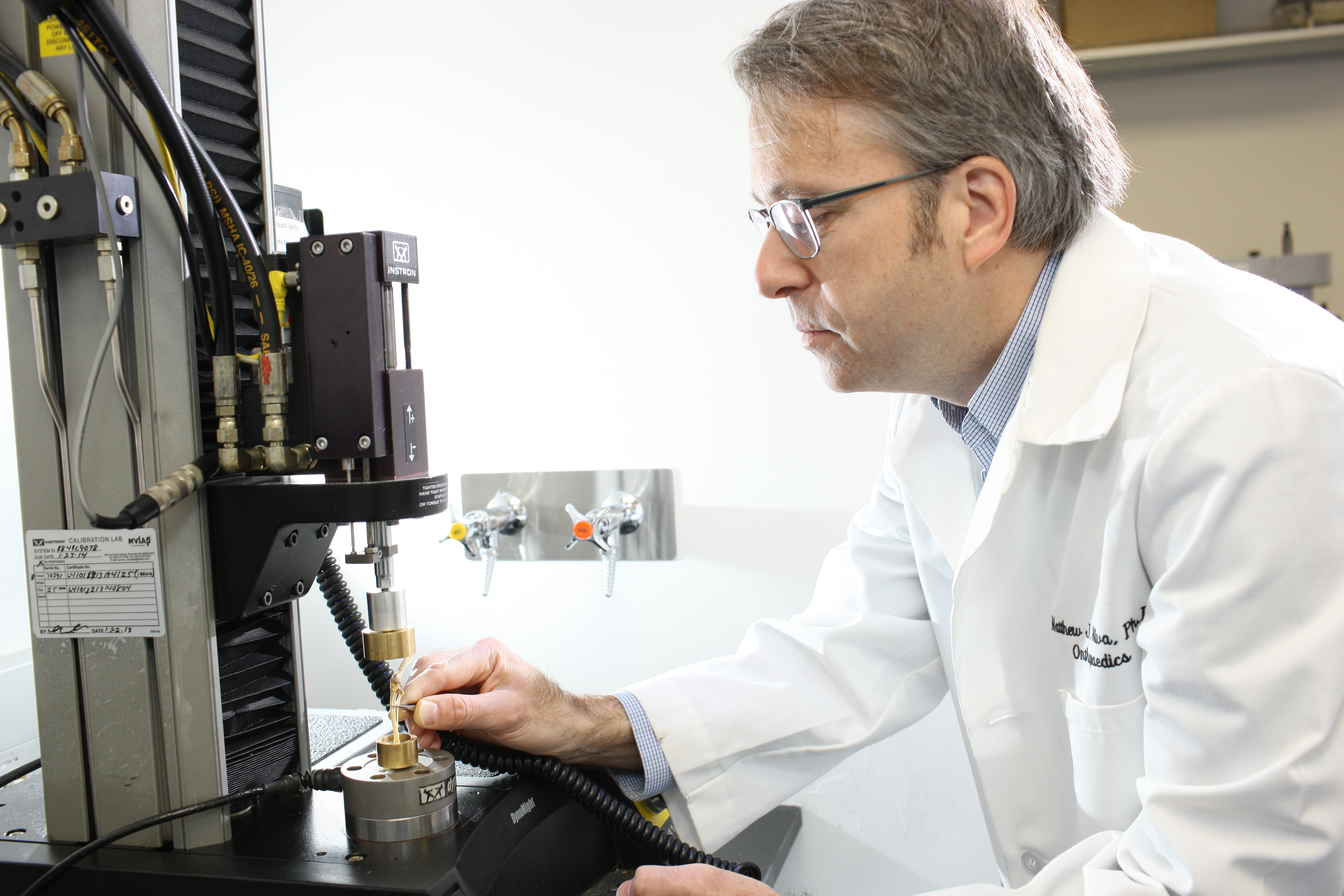 Matthew Silva, PhD, the Julia and Walter R. Peterson Professor of Orthopedic Surgery, is conducting research to better understand which particular cells in the bone are essential for fractures to heal properly, and will use this knowledge to test new ways to accelerate healing in fractures that heal poorly (“nonunions").
Matthew Silva, PhD, the Julia and Walter R. Peterson Professor of Orthopedic Surgery, is conducting research to better understand which particular cells in the bone are essential for fractures to heal properly, and will use this knowledge to test new ways to accelerate healing in fractures that heal poorly (“nonunions").
Fractures are very common in the general population, as well as in members of the military. Fractures that heal poorly lead to prolonged disability and can require multiple surgeries to treat. Approximately 5-10% of fractures heal slowly or not at all and require additional treatment.
Noncombat injuries impact soldier health and fitness for deployment. Musculoskeletal injuries are the most common type of injury, with bone fractures and stress fractures being common in military populations, especially during high-intensity training. In addition, musculoskeletal injuries sustained during combat can result in massive bone loss and require advanced treatments.
Dr. Silva shares, "We anticipate identifying cells in bone that are essential for fractures to heal properly. This is a critical question in fracture healing research. With this information we will explore new ways to “turn on” these cells to accelerate fracture healing. We are grateful to the DOD for supporting our research and proud to do our small share to help our soldiers and veterans."
Be Treated by the Best
Washington University's orthopedic specialists are national leaders in the diagnosis and treatment of children, adults and athletes of all ages. For questions about our research, or to schedule a visit: