- Home
- Education
- Case Studies
- Case Study: Adult Degenerative Lumbar Scoliosis
Case Study: Adult Degenerative Lumbar Scoliosis
A 73-year old woman had lived with scoliosis for decades of her life, symptom free and comfortable. With time, however, she noticed that she was losing height and her head was shifting to the right. Over the course of the past year, in addition to the change in her appearance, she complained of increasing back and leg pain. Nonoperative care failed to offer her any substantial relief, and she found that her most comfortable position was lying down, which led her to do less of the activities she enjoyed in the past. An evaluation by a surgeon led to the recommendation of a two-day surgery, fusing the majority of her spine.
She came to Washington University Orthopedics for a second opinion, provided by Michael P. Kelly, MD, MSc. Dr. Kelly is an Associate Professor of Orthopaedic Surgery and Neurologic Surgery at Washington University, and his practice focuses specifically on spinal deformities in both pediatric and adult patients. A review of her radiographs found degeneration of her lumbar spine, with instability causing compression of lumbar nerve roots. In addition to scoliosis, the degeneration had led to a loss of curvature in the lateral plane, leading to a flat-back which makes standing upright and walking more difficulty due to the energy required to do so.
A discussion ensued regarding possible surgical interventions, ranging from minimally-invasive single level fusions to more extensive, multi-level fusions. A nerve root block failed to identify a single culprit for her pain complaints and a single-level surgery was ruled out. Therefore, a multi-level surgery was indicated as the appropriate surgery.
Washington University Orthopedics has recently published a National Institutes of Health-funded study regarding the care of adult scoliosis patients1, providing excellent information regarding the prognosis of this disease and the outcomes of the various treatment options available to patients.
Multi-level, adult, degenerative scoliosis surgeries are complex, yet increasingly common with the aging patient population. Given the magnitude of these surgeries, it is important for both the patient and the surgeon to be informed regarding the risks, benefits, and expected recovery process for these surgeries.
Through the vision of Keith H. Bridwell, MD, the Spine Division at Washington University Orthopedics has developed a world-renowned adult and pediatric spinal deformity service. Jacob M. Buchowski, MD, MS, Chief of Service, Munish C. Gupta, MD, and Michael P. Kelly, MD, MSc, currently lead the efforts of this service, performing more deformity surgeries annually than most other major academic medical centers. They routinely travel the world to teach the techniques needed for caring for these complicated patients.
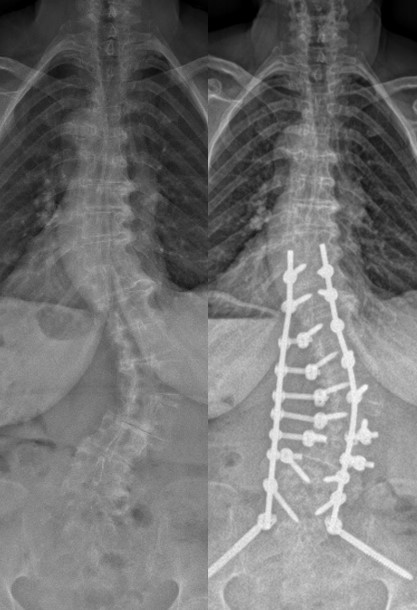 The decision was made to proceed with a single-day surgery fusing the lower thoracic spine to the lumbar spine and sacrum; half the surgery previously offered to the patient. She had a routine 6-day hospital stay, without requiring time in an intensive care unit, and was discharged to a rehabilitation facility to complete her early recovery. She is now without leg pain, standing upright, and happy with the results of surgery.
The decision was made to proceed with a single-day surgery fusing the lower thoracic spine to the lumbar spine and sacrum; half the surgery previously offered to the patient. She had a routine 6-day hospital stay, without requiring time in an intensive care unit, and was discharged to a rehabilitation facility to complete her early recovery. She is now without leg pain, standing upright, and happy with the results of surgery.
1Kelly MP et al. Operative versus nonoperative treatment for adult symptomatic lumbar scoliosis. The Journal of Bone & Joint Surgery, Feb. 20, 2019.
More information: