Anterior Cruciate Ligament (ACL) Tears

Your knee and the ACL
Knee anatomy
 ACL stands for anterior cruciate ligament which is one of the four major ligaments of the knee. It is a strong ligament, that allows you to pivot, twist, and turn. The main function of the ACL ligament is to connect a bone to a bone. In the case of the ACL, this important ligament directly connects the femur (thigh bone) to the tibia (shin bone). In doing so, it prevents these two bones from separating and keeping the tibia from sliding too far forward.
ACL stands for anterior cruciate ligament which is one of the four major ligaments of the knee. It is a strong ligament, that allows you to pivot, twist, and turn. The main function of the ACL ligament is to connect a bone to a bone. In the case of the ACL, this important ligament directly connects the femur (thigh bone) to the tibia (shin bone). In doing so, it prevents these two bones from separating and keeping the tibia from sliding too far forward.
How is the ACL injured?
In the United States, approximately 1 in 3000 people tear their ACL each year. These injuries are very common in an athletic population such as soccer, basketball, and football. These sports require athletes to make vigorous and repeated motions that work the ACL, putting it under stress as it continuously provides stability during stop-and-go action and pivoting motions.
Many injuries to the ACL occur when an athlete initiates a sudden turn or “cut”, but the foot stays planted on the court or ground. Landing from a jump with a twisting motion, as might happen in volleyball or basketball, also can injure the ACL, as well as a hyperextension of the knee and deceleration. However, a direct blow to the outside part of the knee is frequently seen in football players due to the nature of contact experienced by these athletes. Once an athlete sustains an ACL injury, he or she is unlikely to return to competition that day.
Studies show that females are up to eight times more likely to injure their ACL than males. There have been a variety of theories put forth to explain this phenomenon. Most recent research suggests that females have altered firing patterns to their lower extremity muscles during athletic activity that predisposes them to tear their ACL.
Symptoms and diagnosis
The signs that you may have damaged or torn your ACL include:
- A noise like a “pop”
- Pain at the joint, especially with walking or bending
- Immediate swelling
- A feeling of instability in the knee
 Swelling can develop significantly over the first 6 hours after the injury due to bleeding within the knee joint. These are often not isolated injuries, as athletes who tear their ACL experience concomitant damage to the knee cartilage approximately 50%-60% of the time.
Swelling can develop significantly over the first 6 hours after the injury due to bleeding within the knee joint. These are often not isolated injuries, as athletes who tear their ACL experience concomitant damage to the knee cartilage approximately 50%-60% of the time.
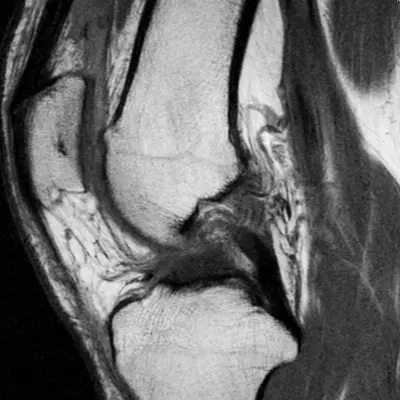
The diagnosis of an ACL tear can typically be made by an experienced sports medicine specialist based on the players history of the injury and physical examination. The most accurate method physicians use to diagnose an ACL tear is the Lachman test that reveals increased motion of the tibia relative to the femur with the knee in a slightly flexed position. Imaging studies are routinely obtained by the treating physician when an ACL tear is suspected. Despite the fact that plain x-rays are usually normal, magnetic resonance imaging (MRI) can be a valuable aid in making the diagnosis and identifying associated injuries.
_____________________________________________________________________________________________________________________
Image (above right) shows MRI of a torn ACL
______________________________________________________________________________________________________________________
Treatment options
Nonsurgical treatment
Athletes who attempt nonoperative management and continue to play sports with a chronic ACL tear frequently develop persistent knee instability which presents as a shifting sensation. They may also complain of swelling or locking which makes return to high-level sports that involve cutting and pivoting very difficult. This instability has been shown to result in cartilage damage in over 90% of patients if left untreated.
People who choose not to have surgery to repair a torn ACL usually do not participate in sports or activities that involve running, twisting, cutting or jumping, or in aggressive activities that place stress on the knee. Nonsurgical management in these types of individuals often does not result in further symptoms. Therefore, activities such as golf, cycling, swimming, and walking can usually be performed despite the presence of an ACL tear in these less active patients.
By undertaking a rehabilitation program, it is possible to function normally without having surgery to reconstruct a torn ACL. Those who foresee only occasional recreational activity may choose rehabilitation over reconstruction. If your lifestyle permits and you elect not to have surgery,
you will be referred to a physical therapist for the development of a plan that will strengthen the knee joint, build your range of motion, control swelling and pain and return you to a normal walking gait.
Surgical treatment
Most often, surgery is required to replace a torn ACL to reestablish normal knee stability. Attempts to directly repair a torn ACL by suturing the fibers back together have proved unsuccessful due to the ligaments inability to heal. Instead, surgeons introduce another piece of tissue, called a graft, that will serve as your new ACL and replace the torn ligament.
The tissue that is harvested to serve in this role can be either an autograft (your own tissue) or an allograft (tissue from another donor). Autografts most commonly come from the tendon that connects your kneecap to the bottom leg bone (the patellar tendon) or from your hamstring tendons. Allografts can come from the patellar tendon or other soft tissue such as the Achilles tendon or the hamstring. The choice of graft tissue is dependent upon several factors that the surgeon will discuss with the patient preoperatively. Overall outcomes, regardless of graft choice, ve been favorable.
Modern reconstructive techniques are performed on an outpatient basis, and the complete surgery typically takes about an hour depending on any coexistent injuries. Surgery will be performed using a minimally invasive technique that employs an arthroscope — a modern tool that requires only tiny incisions to be made. These small incisions serve as ports through which the surgeon inserts long, thin instruments. Tunnels are formed in the bones, and the ends of the graft are placed in the tunnels and affixed to the bones to stabilize them while healing occurs. The articular cartilage and meniscus in your knee will be examined and may require surgical repair or removal as to be determined by your surgeon. If you are scheduled for an upcoming surgery, view our ACL surgical guide for preoperative and postoperative instructions.
Recovery and outlook
Postoperative rehabilitation
After your surgery, you will receive pictures of your surgery, a written instruction sheet customized for your situation, and a set of rehabilitation guidelines. This information will answer most of your questions about recovery.
You will be scheduled to begin physical therapy sometime between 48 and 72 hours after your surgery. At an initial visit with your physical therapist, you will receive training in the exercise program developed for you. You will also learn how to care for your wound and how much weight you should place on the leg.
Your physical therapist will also work with you to set goals for your rehabilitation. How soon your leg will be able to bear weight depends in part on whether your surgeon has performed a meniscus repair in addition to the ACL reconstruction.
Complete rehabilitation will take 5 to 6 months. At the beginning, your progress will be closely monitored, and you will be coached about the right way to do your exercises. As you progress, you will be able to do more of the exercises on your own. If you have any questions at all, you should contact your rehabilitation team.
Returning to work and sports
When you will be able to return to your favorite sport or activity depends, in part, on what the activity is. Also in the equation is your physiology, or physical constitution and structural makeup, over which you have no control. It controls the speed at which you heal.
The most important thing you can do is carefully follow the exercise regimen designed to strengthen your leg. After enough time has passed for you to heal and after you have restored your leg strength, you should be able to return to the physical activity of your choice.
However, you should be aware that surgery does not always completely correct instability. Your doctor will recommend any lifestyle changes that he or she believes are necessary.
After you have regained your strength and eliminated most of your pain, it is important to continue to pursue a physical fitness program with an emphasis on orthopedic health and strength. You should develop a lifelong plan for physical activity that takes into account both muscle strength and aerobic conditioning. An exercise plan will help you prevent future complications. Ask your rehabilitation team for advice.