February 15, 2024
Restricted physical abilities like limb weakness and difficulty gripping or holding things are among the most common obstacles patients face after a stroke. Washington University Orthopedics physical medicine and rehabilitation specialists collaborate with neurosurgeons to offer expert care, including some of the latest technology in the field with vagus nerve stimulation.
The vagus nerve is the longest nerve in the body and the superhighway of the nervous system. It sends messages between your brain and many parts of the body.
What is a Vagus Nerve Stimulator?
A vagus nerve stimulator (VNS) can be used to reduce upper extremity motor deficits and improve motor function in stroke patients with moderate to severe arm impairment. The system consists of an implantable pulse generator (IPG), an implantable lead, programmable software, and a wireless transmitter. The non-rechargeable device is implanted just under the skin with 2 small incisions during a same day outpatient procedure. The lead runs from the left vagus nerve in the neck to the IPG in the chest. The technology is intended to stimulate the vagus nerve while a rehabilitation movement occurs.
Who does VNS help?
Vagus nerve stimulation can benefit patients who are still suffering from upper limb hemi- or monoplegia post-stroke, who have gone through standard outpatient therapy approaches and clinical evidence no further improvements can be made from standard care. Stroke survivors have experienced two to three times more hand and arm function with the implementation of vagus nerve stimulation in their rehabilitation regimens.
How does it work?
-
A small device is surgically implanted under the skin in the upper left chest area during an
outpatient procedure. Patients return home the same day.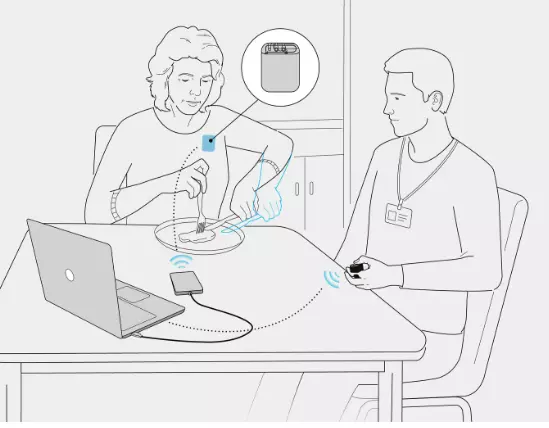
- One week after implantation, the stroke survivor restarts upper-limb occupational and physical therapies. A therapist will activate the device to signal delivery of a gentle pulse to the vagus nerve while the patient performs specific tasks. Pairing exercise with VNS releases neuromodulators that create and strengthen neural connections to improve upper limb function.
- Users will learn how to activate the system at home during rehab exercises and routine tasks. VNS during daily activities, such as folding laundry, preparing a meal or getting dressed, helps stroke survivors improve what matters most to them.
Nearly 60% of stroke survivors suffer from impaired upper limb function. Vagus nerve stimulation offers safe and effective intervention for those who have not yet regained hand and arm mobility, even years later.