- Home
- Patient Care
- Services
- Shoulder & Elbow
- Overview
- Rotator Cuff
- Rotator Cuff Surgery
Rotator Cuff Surgery
Rotator Cuff Surgery
The rotator cuff surgery you have been scheduled for is to correct the problems that you have been having in your shoulder. Your doctor has discussed with you the possible surgeries that may assist in helping correct your problems. You surgery could include the following:
Rotator Cuff Repair
A rotator cuff repair involves reattaching the end of the torn tendon to the bone. This can, in the majority of cases, be performed as an arthroscopic outpatient procedure. An arthroscopic rotator cuff repair requires a few small (1 cm or less) incisions. We make a small incision in the back of the shoulder and a camera is placed inside the shoulder joint. We make a small incision in the front of the shoulder and working instruments are placed through this incision. We examine all the structures in the shoulder at the time of surgery and address any problems that we may see. The camera is then repositioned above the rotator cuff and another incision is made on the side of the shoulder. Instruments are used to remove the inflamed bursa.
The rotator cuff tear is then repaired: One or two small incisions are made on the top of the shoulder in order to place anchors. Anchors look like very small screws that have an eyelet through which a couple of sutures are passed. The anchors are placed into the bone where we plan to reattach the tendon. Instruments are used to pass the sutures through the tendon and knots are tied restoring an anatomic tendon insertion to the bone. The number of anchors required depends on the size of the tear. In some cases of larger cuff tears or tears in front of the rotator cuff tendon, an open (larger incision) may need to be performed. This decision is made at the time of surgery.
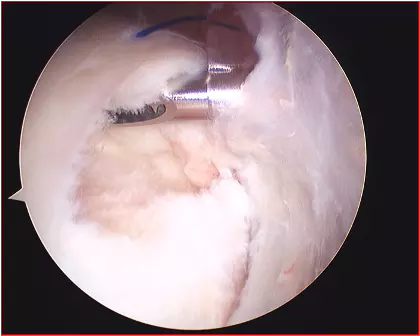
Above: Rotator Cuff Tear

Above: Surgically Repaired Rotator Cuff
Subacromial Decompression
A subacromial decompression involves removal of inflamed tissue within the space above the shoulder joint between the rotator cuff and the acromion which is part of the shoulder blade on the top of the shoulder. If there are any bone spurs present, we smooth them with a small burr. This is a standard part of rotator cuff surgery.
Biceps Tenotomy or Tenodesis
Surgery for a diseased biceps tendon is needed in about 25% of patients with a rotator cuff tear. A
biceps tendon procedure is only performed if there is a problem with the biceps tendon which is felt to
be significant enough to remain a source of shoulder pain after rotator cuff surgery. Sometimes, biceps
disease is not seen until the time of surgery, as damage is not always seen on a MRI or ultrasound.
Surgery for a torn biceps tendon involves removing it from inside the joint and reattaching it where it exits the joint. In some cases, we simply cut the tendon and allow it to retract from the joint. The negative consequences of this procedure are possible asymmetry of the biceps muscles (that it will look different from side to side) and possibly some spasm in the muscle belly which routinely resolves. This rarely causes a problem, and removing the long head of the biceps tendon from the shoulder does not affect shoulder function. The biceps muscle continues to work at the elbow and moving or releasing this tendon does not affect motion or strength of the shoulder.
Sometimes a biceps tenodesis can be performed arthroscopically. However, in younger or more active patients, an open biceps tenodesis surgery may be recommended. Your surgeon will discuss this with you prior to surgery.
Distal Clavicle Resection
A distal clavicle resection is performed if there is pain at the acromioclavicular joint. The decision to perform a distal clavicle resection is based on symptoms. Many patients have changes of this joint on radiographic studies (x-rays or MRI).
If the joint is not painful, there is no reason to perform surgery on it, regardless of x-ray/MRI reports. If the joint is painful, surgery is performed to debride the joint and remove about 5-7 mm of the bone. The ligaments are left attached to preserve stability, and there is no loss of shoulder function. Performing a distal clavicle resection will not lengthen your recovery period.
Preoperative Planning
Depending on the location of your surgery it may be required to have preoperative testing. In some cases blood work, EKG (heart tracing), or a chest X-ray may be needed. If any of these tests are needed they will be scheduled for you and will be done during pre-testing when you meet with the anesthesia staff. If it has been some time since you have seen your primary care physician and you have several medical problems, it would be best that you see your primary care physician before your pre-test date.
Night Before Surgery
You should not have anything to eat or drink after midnight the night before surgery. You may be advised to take some of your medications with a sip of water only. The anesthesia staff will discuss this with you at the time of your pre-testing.
Arriving at the Hospital
You will arrive at the hospital approximately two hours before your scheduled surgery time. Occasionally, a procedure scheduled ahead of yours may take longer than expected, so there may be some delay before your surgery. Regardless, it is important that you arrive on time.
Before Surgery
Upon arrival to the hospital, you will go through a check-in process. A nurse will see you, review your records, and an IV will be started. A member of the anesthesia team will meet with you to discuss any anesthesia concerns and anesthetic options. Your surgery will be performed under general anesthesia (you will go to sleep.) In addition, the anesthesiologist may recommend a regional block if they think that you are a good candidate. This involves an injection of local anesthetic (numbing medicine) or placement of a catheter near the nerves at the base of the neck. These blocks are generally recommended to help control your pain following surgery. The anesthesiologist will discuss the risks of the block. The decision to perform this is a mutual decision between the patient and the anesthesiologist.
During Surgery
You can anticipate that your surgery will last approximately 1 ½ to 2 ½ hours, although this varies from case to case. Your belongings will be stored in a locker in the pre-operative area. If you have family members with you they will wait for you in the waiting room. During your surgery, family members should plan on remaining in or near the waiting area in order to be accessible at the completion of the procedure. Your surgeon will speak with them immediately after your surgical procedure to let them know that you are finished.
After Surgery
When you wake from surgery you will be located in the post-operative recovery room. Once you have been stabilized and are comfortable, family members will be invited to sit with you while you continue recovering from surgery. You will have a dressing on your shoulder and your arm will be immobilized in a sling. To be discharged to go home, your pain should be under control,and you should be eating, drinking, and able to walk to the bathroom with minimal assistance.
>>Next topic: Postoperative Care