Total Shoulder Replacement (Arthroplasty)
Why have a shoulder replacement?
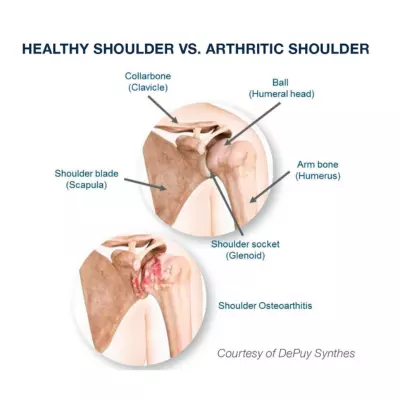 Total shoulder arthroplasty is a joint replacement surgery for a variety of painful shoulder joint conditions – most commonly osteoarthritis of the joint. Osteoarthritis is a condition where the cartilage degenerates leading to bone on bone contact and spur formation around the joint. This leads to pain, stiffness and decreased shoulder function.
Total shoulder arthroplasty is a joint replacement surgery for a variety of painful shoulder joint conditions – most commonly osteoarthritis of the joint. Osteoarthritis is a condition where the cartilage degenerates leading to bone on bone contact and spur formation around the joint. This leads to pain, stiffness and decreased shoulder function.
Other conditions that may require a shoulder replacement include:
- Rheumatoid arthritis
- Post-traumatic arthritis
- Avascular necrosis (osteonecrosis)
- A previous shoulder replacement that was not successful
- Failure of conservative treatments such as anti-inflammatories, cortisone injections, or physical therapy
The primary reason to consider a shoulder replacement is pain relief. Generally, there is also an improvement in shoulder range of motion and function as well.
Why have a reverse shoulder replacement?
Reverse total shoulder arthroplasty is a joint replacement surgery for a variety of painful shoulder conditions, where the rotator cuff tendons are badly damaged and beyond repair or there is severe destruction of the socket (glenoid bone). Severe rotator cuff problems can occur in association with:
- Arthritis
- Shoulder instability
- Certain fractures
- Failure of a previous joint replacement or failed rotator cuff repair surgery
Reverse shoulder replacement surgery changes the mechanics of the shoulder transferring more load to the deltoid muscle and less load to the rotator cuff muscles for adequate function. The best clinical results for a reverse replacement are seen in patients who have some functioning rotator cuff tendons/muscles; however, very good results can be seen even with large rotator cuff tears.
In the reverse total shoulder the ball and socket are replaced, but they are reversed. The socket portion of your shoulder is replaced with a prosthetic metal ball that attaches to a metal baseplate secured to the socket/scapula. The humeral head (ball portion) of your shoulder is replaced with a plastic cup that is attached to the top of a metallic stem placed within the humerus (the upper arm bone).
 How does the shoulder work?
How does the shoulder work?
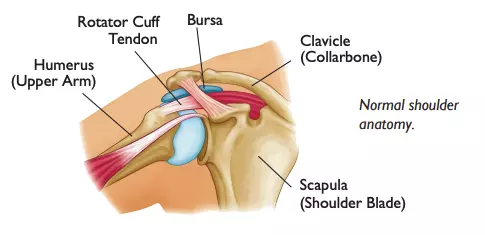
The shoulder is made up of two joints, the acromioclavicular joint and the glenohumeral joint, muscles, ligaments and tendons.
- The acromioclavicular joint is where the acromion, part of the shoulder blade (scapula) and the collar bone (clavicle) meet.
- The glenohumeral joint is where the ball (humeral head) and the socket (the glenoid) meet.
- The rotator cuff connects the humerus to the scapula and is made up of the tendons of four muscles. Tendons attach muscle to bone. The deltoid muscle is the muscle that forms the rounded curve of the shoulder. Muscles in turn move bones by pulling on the tendons. The muscles of the rotator cuff keep the humerus tightly in the socket.
- The socket, or the glenoid, is shallow and flat. It is rimmed with soft tissue called the labrum that makes a deeper socket that molds to fit the humeral head.
- The joint capsule surrounds the shoulder joint. It is a fluid-filled sac that lubricates the joint. It is made up of ligaments. Ligaments are soft tissue that holds bone to bone. Shoulder injuries can occur to any part of the shoulder.
How can surgery help?
 During anatomic shoulder replacement, the ball and socket portion of your shoulder will be replaced with metal and plastic parts that are similar in shape and size to your own shoulder anatomy – hence the name “anatomic”. The socket portion of your shoulder is resurfaced with a plastic socket and the ball portion (humerus) is replaced with a metal ball attached to a metal stem of various lengths secured within the humerus.
During anatomic shoulder replacement, the ball and socket portion of your shoulder will be replaced with metal and plastic parts that are similar in shape and size to your own shoulder anatomy – hence the name “anatomic”. The socket portion of your shoulder is resurfaced with a plastic socket and the ball portion (humerus) is replaced with a metal ball attached to a metal stem of various lengths secured within the humerus.
Pictured to the right: X-ray of an anatomic total shoulder replacement. Please note that this image doesn't reflect the exact type of an implant used by the surgeon.
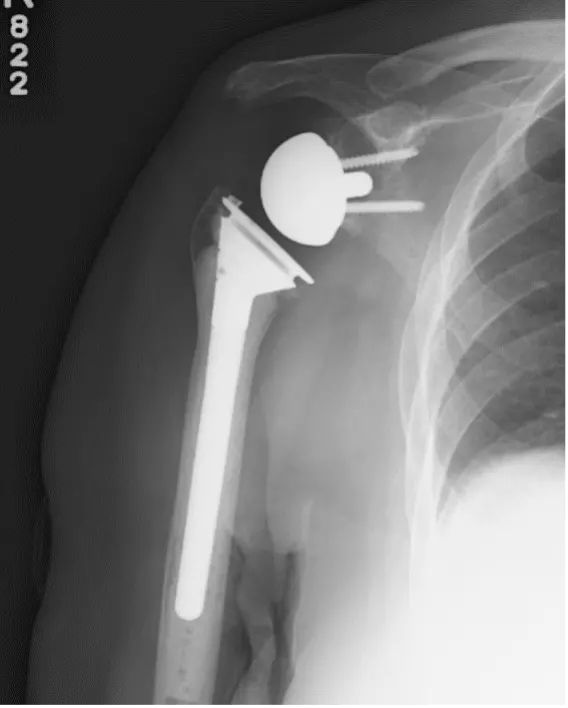 In a reverse total shoulder replacement, the ball and socket are replaced, but they are reversed. The socket portion of your shoulder is replaced with a prosthetic metal ball that attaches to a metal baseplate secured to the socket/scapula. The humeral head (ball portion) of your shoulder is replaced with a plastic cup that is attached to the top of a metallic stem placed within the humerus (the upper arm bone).
In a reverse total shoulder replacement, the ball and socket are replaced, but they are reversed. The socket portion of your shoulder is replaced with a prosthetic metal ball that attaches to a metal baseplate secured to the socket/scapula. The humeral head (ball portion) of your shoulder is replaced with a plastic cup that is attached to the top of a metallic stem placed within the humerus (the upper arm bone).
Pictured to the right: X-ray of a reverse total shoulder replacement. Please note that this image doesn't reflect the exact type of an implant used by the surgeon.
Expected outcomes
Anatomic shoulder arthroplasty has been performed in the United States since the 1950’s. At that time, it was used to treat severe shoulder fractures. In recent years, this surgery has become more common and is used for many painful shoulder conditions. Anatomic replacement is very reliable for pain relief and improvement in shoulder range of motion and function in over 95% of patients. It is expected that an anatomic replacement will last 12-15 years in over 80% of patients. Our shoulder surgeons perform about 650 total shoulder replacement surgeries each year.
Reverse shoulder arthroplasty has been performed in the United States since 2004. Therefore, long-term outcomes and risks of long-term complications are not known at this time. This surgery is reliable for pain relief in over 90% of patients. While some patients have complete relief of pain, most experience mild activity related pain in the shoulder and down the arm. This is generally felt to be muscular pain and is usually mild. Most patients will also have an improvement in the ability to raise the arm overhead but this is somewhat dependent on the age of the patient, the strength of the deltoid muscle and the presence of some remaining rotator cuff tissue.
It is realistic to expect to be able to raise the arm above shoulder level, to reach the top of the head and the opposite shoulder in most patients. Your ability to rotate the arm outward is dependent on the presence of some intact rotator cuff tendon as well. The reverse also improves strength when lifting away from the body. After a reverse shoulder replacement, some patients will lose some motion reaching behind the back. Most patients will be able to reach their belt line or back pocket but some can go a little higher. For patients with shoulder dislocation problems, shoulder stability is reliably restored. However, the risk of early dislocation following a reverse shoulder replacement is slightly greater than a standard replacement and can occur in up to 2-3% of patients.
Most patients can very active after recovering from an anatomic or reverse shoulder replacement. You can golf, play tennis, swim, hunt, do light yard work and garden. We recommended that patients do not routinely lift more than 25 pounds overhead after surgery, but there are no lifting and push/pull restrictions below shoulder height. Patients with shoulder replacements can perform light and medium demand labor jobs; however, it is not designed for sustained heavy manual labor. You can lift lighter weights with higher repetitions. Long-term durability of the reverse replacement is not known; the more you take care of your shoulder the longer it will likely last.
Getting Ready for Surgery
Schedule an appointment with your primary care provider and dentist if you haven’t been evaluated within the last year. Complete your dental work before the shoulder surgery. To make sure it is safe for you to have anesthesia for your surgery, you will meet with our anesthesia specialists 2-3 weeks before surgery. Your surgeon may also recommend advanced imaging studies such as an MRI or CT scan of the shoulder to help with surgical planning. For more information, refer to the journey guide.
Your surgery and hospital stay
Postoperative recovery
After surgery your shoulder will be placed in a sling for 2-3 weeks. Depending on the surgeon’s preference, the dressing can be removed in 1-2 weeks.
You will begin your exercises the morning after surgery. These exercises will be done 3-4 times per day while in the hospital and at home. Supervised physical therapy may be recommended by your surgeon starting 3-6 weeks after the surgery.
Learn more by downloading our total shoulder replacement journey guide, which has more information on surgery preparation and postoperative recovery.
Common Questions and Answers
What restrictions will I have after surgery?
- No weight bearing through the arm – this means do not push or pull with your operative arm to get out of the bed or up from a chair.
- Do not attempt to reach behind or up your back.
- Although we recommend that you wean from your sling within a couple of weeks and begin to use your arm, do not lift more than a cup of coffee with the operative arm for 6 weeks.
- Please refrain from any dental, bladder or bowel procedures for 3 months following surgery. Once
you are 3 months out from surgery you will need to be pre-medicated with antibiotics prior to any of these procedures for 2 years from the date of surgery.
How long does the surgery last?
About 1.5-2 hours. Your surgeon will discuss whether you are a candidate for a same day discharge, or if a one night hospital stay is the best option for you.
How long is the recovery?
Full recovery takes about 3-6 months.
When can I…?
- Drive: You should wait until after your first postoperative visit, about 2 weeks from surgery.
- Return to work: If you have a light duty or desk job, you may return to work as soon after surgery as you feel comfortable. Physically demanding jobs may require 6 weeks to 6 months of recovery before returning to work.
- Play tennis, golf or other active sports: around 4 to 6 months from surgery.
- How often do I see my surgeon after surgery? You will have 3-5 follow up appointments during the first 6 months after the surgery. Annual follow up appointments are very important. We will take X-rays to check the following:
- The amount of bone ingrowth.
- The position of the implant.
- The condition of the bone around the prosthesis.
Problems from Surgery
Although shoulder replacement can help with pain, there’s also the chance that surgery will cause problems. These problems are called complications.
The list below includes some of the most common complications from this surgery. Fortunately, complications are very rare. Please note that this list includes some, but not all, of the possible side effects or complications. In some cases, such as infection, further surgery may be needed to treat the problem. Some complications will resolve or improve with time. There are also risks associated with general anesthesia that are dependent on your overall health.
- Infection: 1% risk, can occur early or late
- Dislocation: 1-3% risk, rare after the initial 6 weeks
- Vascular (blood vessel) injury: very rare
- Hematoma/excessive swelling: 5% risk
- Nerve complication: up to 10%, these are partial injuries from nerve irritation and resolve in 95% of cases over time
- Blood clots in legs or lungs: clots that cause symptoms are seen in 1-2% of cases despite steps taken to prevent these. Please let your surgeon know if you have a personal or family history of blood clots.
- Persistent shoulder pain and stiffness
- Revision surgery: Any time prosthetic components (man made parts) are put into a joint, there is always a very small chance that one or more of the parts may have a problem that requires another surgery in the future.